For home health agencies, when hiring medical directors and employees, it is critical to consistently check your employees on the OIG, SAM and state exclusion sites to ensure no prior history.
An OIG analysis of Medicare claims filed in 2014 and 2015 reveals high prevalence of fraud, particularly in certain geographies spread out in 12 states.
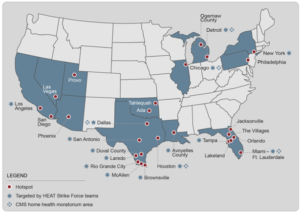
Source: https://oig.hhs.gov/oei/reports/oei-05-16-00031.asp#
The analysis noted that over 4500 physicians in these geographies were found to have acted irregularly as compared to their counterparts in other parts of the country. Some of the irregularities noted include:
- Paying for patient referrals.
This act contravenes the Federal anti-kickback statute that forbids direct or indirect payment by HHAs to physicians for referrals. The same statute also forbids physicians from soliciting or accepting payments for referrals.
- Billing where medical services have not been given or for services that are medically unnecessary. Some physicians also falsified patients’ status as home bound
Physicians who perform these acts violate the statutes that govern health-care fraud and prohibit giving false statements on matters related to health care.
OIG’s response to health care fraud
To deter fraudulent physicians, emphasis has been laid on the need for continued vigilance and scrutiny in home health care through increased evaluations, audits, arrests and enforcement actions by OIG, law enforcement officials and Centers for Medicare & Medicaid Services (CMS).
In June this year, OIG, with the assistance of law enforcement officials arrested 300 people from 36 districts who were subsequently charged with falsely billing around $900 million to Medicare and Medicaid.
Past investigations carried out between 2011 and 2015 by OIG and US government accountability office resulted in over 350 civil and criminal convictions of fraud-related cases and recovery of more than $975 million dollars.
These efforts are expected to reduce cases of improper conduct, illegitimate compensation arrangements, issues of non-compliance and questionable billings & payments. Estimates also show that the payoff of takedowns and convictions is worth for taxpayers as each $1.00 of taxpayer money spent to fight fraud in health care recovers $6.10.
HHAs and Physicians Are Urged to be vigilant
An alert issued by the Office of Inspector General (OIG) on June 22, 2016, points out that fraud in health care has serious implications, some of which include:
- Substantial increases in costs incurred by health care programs
- Encouraging unfair competition
- Promoting dishonest medical judgement
- Increased cases of patient steering, which may result in harm to patients or deny patients of the best possible care.
Health care providers are urged to exercise caution by doing the following:
- Physicians and HHAs should ensure that all compensation arrangements entered into are legitimate and should not be disguised as payments for services purportedly rendered. Payments should also be fair and reflective of market value.
- HHAs should investigate all claims received to confirm patients are home bound.
